PubMed Central, CAS, DOAJ, KCI

Articles
- Page Path
- HOME > J Yeungnam Med Sci > Volume 38(1); 2021 > Article
-
Original article
Association between gestational age at delivery and lymphocyte-monocyte ratio in the routine second trimester complete blood cell count -
Hyun-Hwa Cha
 , Jong Mi Kim
, Jong Mi Kim , Hyun Mi Kim
, Hyun Mi Kim , Mi Ju Kim
, Mi Ju Kim , Gun Oh Chong
, Gun Oh Chong , Won Joon Seong
, Won Joon Seong
-
Yeungnam University Journal of Medicine 2021;38(1):34-38.
DOI: https://doi.org/10.12701/yujm.2020.00234
Published online: June 18, 2020
Department of Obstetrics and Gynecology, Kyungpook National University Hospital, School of Medicine, Kyungpook National University, Daegu, Korea
- Corresponding author: Won Joon Seong Department of Obstetrics and Gynecology, Kyungpook National University Hospital, School of Medicine, Kyungpook National University, 807 Hoguk-ro, Buk-gu, Daegu 41404, Korea Tel: +82-53-200-2686 Fax: +82-53-200-2086 E mail: wjseong@knu.ac.kr
Copyright © 2021 Yeungnam University College of Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 5,589 Views
- 103 Download
- 4 Crossref
Abstract
-
Background
- We aimed to determine whether routine second trimester complete blood cell (CBC) count parameters, including neutrophil-lymphocyte ratio (NLR), lymphocyte-monocyte ratio (LMR), and platelet-lymphocyte ratio (PLR), could predict obstetric outcomes.
-
Methods
- We included singleton pregnancies for which the 50-g oral glucose tolerance test and CBC were routinely performed between 24 and 28 weeks of gestation in our outpatient clinic from January 2015 to December 2017. The subjects were divided into three groups according to their pregnancy outcomes as follows: group 1, spontaneous preterm births, including preterm labor and preterm premature rupture of membranes; group 2, indicated preterm birth due to maternal, fetal, or placental causes (hypertensive disorder, fetal growth restriction, or placental abruption); and group 3, term deliveries, regardless of the indication of delivery. We compared the CBC parameters using a bivariate correlation test.
-
Results
- The study included 356 pregnancies. Twenty-eight subjects were in group 1, 20 in group 2, and 308 in group 3. There were no significant differences between the three groups in neutrophil, monocyte, lymphocyte, and platelet counts. Although there was no significant difference in NLR, LMR, and PLR between the three groups, LMR showed a negative correlation with gestational age at delivery (r=−0.126, p=0.016).
-
Conclusion
- We found that a higher LMR in the second trimester was associated with decreased gestational age at delivery. CBC parameters in the second trimester of pregnancy could be used to predict adverse obstetric outcomes.
- Preterm birth is a major cause of long-term morbidity and mortality in infants. Therefore, there have been many studies about the etiology and pathophysiology of preterm birth and methods for its early prediction and prevention.
- Complete blood cell (CBC) count parameters including neutrophil-lymphocyte ratio (NLR), lymphocyte-monocyte ratio (LMR), and platelet-lymphocyte ratio (PLR) have been used for the detection of malignant diseases [1,2] or the prediction of prognosis in various diseases [3-5]. Meanwhile, in pregnant women, CBC for verifying hematocrit or hemoglobin is usually checked between 24–28 weeks during gestational diabetes mellitus (GDM) screening. Although CBC is not a good screening tool for pregnancy-associated diseases, it can provide valuable physiological information regarding pregnant women [6]. Labor is also an inflammatory response; therefore, CBC parameters could be used to predict preterm birth [7]. Recently, several studies have reported the association between CBC parameters and adverse obstetric outcomes such as GDM, hypertensive disorder, and preterm birth [8-12]. However, they were retrospective [8], case-control studies [10], or included cases after threatened preterm labor had developed [12]. This study aimed to determine whether routine second trimester CBC parameters during GDM screening could predict obstetric outcomes in pregnancy.
Introduction
- This prospective observational study was conducted at the Kyungpook National University Hospital, Daegu, Korea, between January 2015 and December 2017 and approved by the Institutional Review Board of the Kyungpook National University Chilgok Hospital (IRB No: 2019-12-009).
- We included singleton pregnancies for which the 50-g oral glucose tolerance test (OGTT) and CBC count with differential count were routinely performed in the outpatient clinic between 24 and 28 weeks of gestation. Pregnant women were divided into three groups according to the pregnancy outcomes as follows: group 1 included preterm births due to preterm labor, preterm premature rupture of membranes (PPROM), or incompetent internal os of the cervix (IIOC). Preterm births were defined as births between 200/7 and 370/7 weeks of gestation. Preterm labor was defined as regular uterine contractions with a cervical change occurring at least three times every 10 minutes before 370/7 weeks of gestation. PPROM was defined as membrane rupture occurring spontaneously without labor before 370/7 weeks of gestation. IIOC was defined as painless cervical dilatation in the second trimester. Group 2 included preterm births due to maternal, fetal, or placental causes (hypertensive disorders including gestational hypertension and preeclampsia (PE), fetal growth restriction which was defined as the estimated fetal weight being suspected in the bottom 10 percentile at the corresponding gestational age, or placental abruption). Group 3 included term deliveries regardless of the indication of delivery. The exclusion criteria were as follows: multifetal gestation, gravidas who had diseases that could influence maternal CBC count levels, including malignant diseases, rheumatoid disorders, chronic hypertension, renal diseases, pregestational diabetes mellitus, or hematologic diseases. We compared CBC parameters between the three groups and evaluated the association of gestational age at delivery with CBC parameters using a bivariate correlation test. Statistical analyses were performed using the IBM SPSS version 19.0 (IBM Corp., Armonk, NY, USA) software. The results were considered statistically significant when the p-value was below 0.05.
Materials and methods
- During the study period, 50-g OGTT and CBC were performed on 577 singleton pregnant women in our outpatient clinic. Among them, 221 did not deliver their babies at our institution. Consequently, we were able to include 356 singleton pregnancies. Forty-eight (13.5%) women delivered their babies before 370/7 weeks of gestation, with 28 (7.9%) being in group 1 and 20 (5.6%) in group 2.
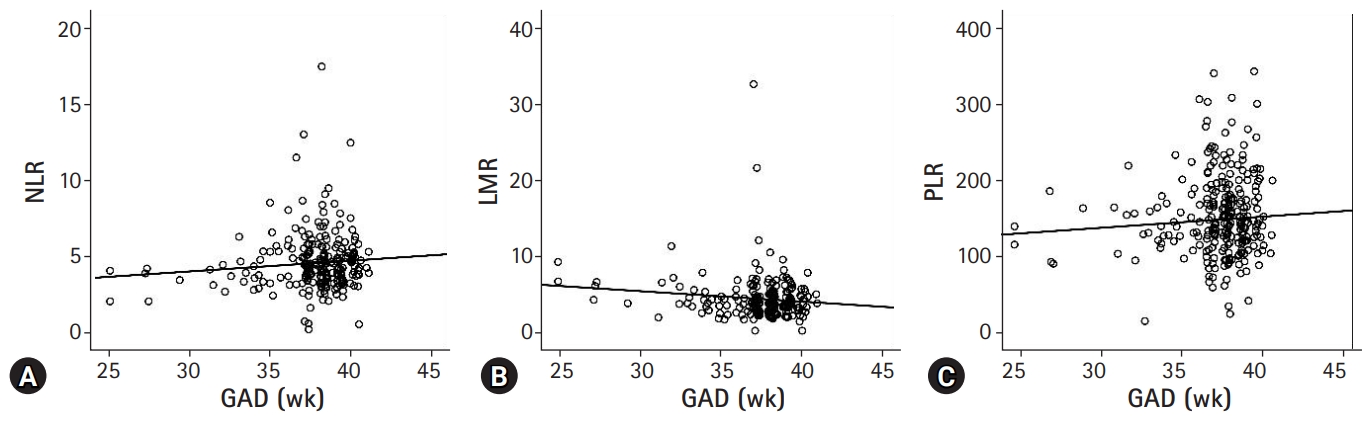
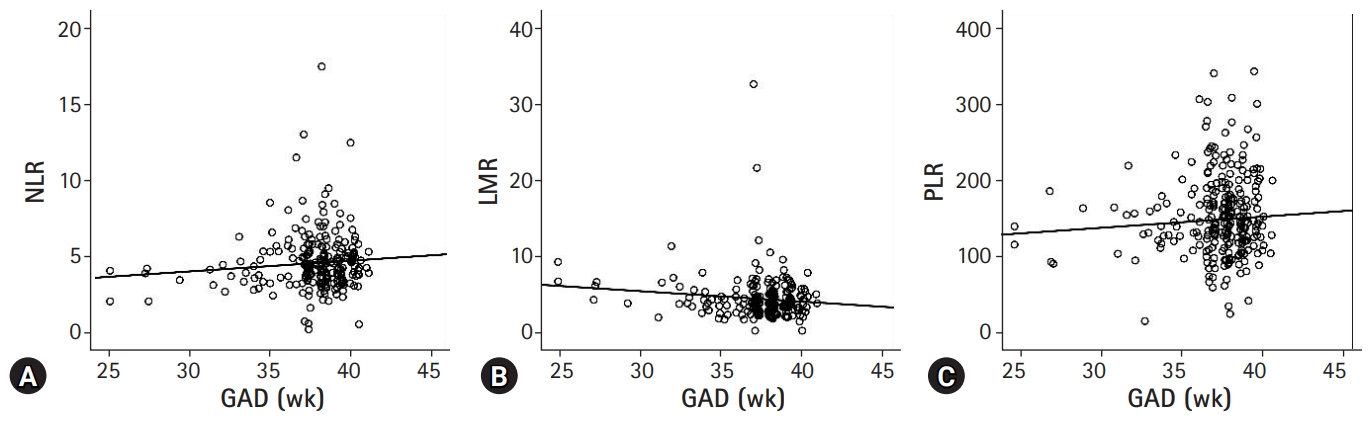
- The maternal and neonatal outcomes are shown in Table 1. There were no significant differences in maternal characteristics except for maternal weight at delivery and the rate of cesarean section. However, neonatal characteristics, including gestational age at delivery, birth weight, and Apgar score, differed between the three groups. The comparison of CBC parameters between the three groups is shown in Table 2. No significant differences were found in neutrophil, monocyte, lymphocyte, and platelet counts. Moreover, there was no significant difference in other CBC parameters including NLR, LMR, and PLR between the three groups. However, we observed a negative correlation between LMR and gestational age at delivery (r=−0.126, p=0.016) (Fig. 1).
Results
- In this study, we compared the CBC parameters that were prospectively obtained from routine GDM screening between 24 and 28 weeks of gestation according to the obstetric outcomes. Although there was no significant difference in CBC parameters according to the obstetric outcomes defined as spontaneous preterm birth, indicated preterm birth, or term delivery, we found that LMR was negatively correlated with gestational age at delivery. Clinically, there seemed to be a positive correlation between NLR and gestational age at delivery (p=0.074). These results suggested that an increased lymphocyte count in the second trimester could be associated with a lower gestational age at delivery.
- Recently, several inflammatory markers including CBC parameters have been identified as predictive factors in various diseases [13,14]. Since labor is also an inflammatory response, the role of inflammatory markers, such as C-reactive protein or CBC parameters, has been assessed in term and preterm labor [7,12,15]. The analysis of inflammatory markers in addition to CBC parameters could be more informative; however, we aimed to obtain information about obstetric outcomes from routine CBC sampling without an additional laboratory test.
- Notably, there have been studies regarding the detection of actual preterm birth in women with threatened preterm labor using CBC parameters [12,16]. Daglar et al. [12] reported that LMR was significantly increased in pregnant women with threatened preterm labor who delivered prematurely than in similar women whose pregnancies continued to term. They also showed a negative correlation between gestational age at delivery and LMR in preterm births. Additionally, Gezer et al. [16] reported that a high NLR value at the time of admission was an independent risk factor for preterm birth in women with threatened preterm labor between 34 and 37 weeks of gestation. We assumed that there had been an increase in neutrophil or lymphocyte counts in the group with true labor. However, these two studies evaluated the role of CBC parameters in women with threatened preterm labor. Unlike these two studies, we prospectively collected maternal CBC parameters during routine 50-g OGTT and enrolled our patients before they had developed threatened preterm labor.
- The differential count of CBC is known to change during normal pregnancy [6,17]. Li et al. [6] established a reference interval for CBC parameters during normal pregnancy in Chinese women showing a decrease in lymphocyte count contrary to the changes in white blood cell count due to the increase in neutrophil count. They suggested the increased neutrophil count was in response to the physiologic stress of pregnancy or impaired neutrophil apoptosis [6,17]. However, they did not comment about the changes in lymphocyte count that decreased during the first and second trimesters of pregnancy and increased in the third trimester. Moreover, they recorded a definitive increase in monocytes during pregnancy [17]. The absence of lymphocyte count reduction or the monocyte count increase observed in a normal pregnancy could imply a decrease in gestational age at delivery.
- LMR has been proposed as a surrogate marker for inflammation and has prognostic value too [18-20]. Further, an abnormal monocyte or lymphocyte count has been shown to have an adverse effect on the prognosis of various diseases [21,22]. In the field of obstetrics, there have been several studies regarding the association between CBC parameters and obstetric complications in addition to the ability of CBC to predict preterm birth. Sargin et al. [8] investigated whether there were differences in the NLR and PLR between glucose intolerance (e.g., GDM patients), impaired glucose tolerance, GDM-screening-positive, and control groups. They concluded that NLR or PLR could not be used for the screening of GDM. However, they also observed that the lymphocyte and neutrophil counts were higher in the glucose-intolerance group compared to those in the control group. However, Mertoglu and Gunay [9] showed differences in NLR and PLR between glucose-intolerance and normal control groups in non-pregnant adults and they suggested that these markers could be used to predict prediabetes and diabetes mellitus. Previous studies have suggested the efficacy of CBC parameters as a prognostic factor in women with PE [10,11]. Gogoi et al. [10] showed that NLR, PLR, red cell distribution width, and mean platelet volume were higher in women with PE in a case-control study. Oylumlu et al. [11] suggested that NLR could be used as a marker for risk stratification in PE patients. We performed subgroup analysis that included indicated preterm birth and term deliveries (group 2 vs. group 3, data not shown), but there was no significant difference between the two groups. Unlike our study, studies by Gogoi et al. [10] and Oylumlu et al. [11] were retrospective or case-control studies that included patients diagnosed as having GDM or PE. Moreover, group 3 in our study group included pregnancies complicated with PE beyond 37 weeks of gestation.
- This study has several limitations that need to be taken into consideration while interpreting the results. Although we observed a negative correlation between LMR and gestational age at delivery, we could not clarify the mechanism underlying this phenomenon. Moreover, our study sample was relatively small, and we did not consider the obstetric complications in pregnancies beyond 37 complete weeks of gestation. However, we think that the most important prognostic factor is the gestational age at delivery. Additionally, we evaluated CBC parameters before the onset of obstetric complications unlike previous studies. Further studies to evaluate CBC parameters considering the changes of those parameters between the second and third trimesters would provide predictive information about perinatal morbidity related to the lower gestational age at delivery or preterm birth.
- Although there was no significant difference in CBC parameters according to obstetric outcomes, we found that a higher LMR in the second trimester was associated with a decreased gestational age at delivery. CBC parameters in the second trimester of pregnancy could be used to predict adverse pregnancy outcomes.
Discussion
-
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
-
Author contributions
Conceptualization: WJS, HHC, GOC; Data duration: JMK, HMK, MJK; Investigation: HHC, JMK, MJK, HMK, GOC; Writing-original draft: HHC; Writing-review & editing: JMK, HMK, MJK, WJS, GOC.
Notes
| Variable | Group 1 (n=28) | Group 2 (n=20) | Group 3 (n=308) | p-value |
|---|---|---|---|---|
| Age (yr) | 32.1±4.2 | 34.1±4.6 | 33.1±4.8 | 0.328a) |
| GAL (wk) | 25.2±1.6 | 25.6±1.4 | 25.0±1.4 | 0.200a) |
| GAD (wk) | 33.7±2.8 | 34.2±3.5 | 38.5±1.1 | <0.001a) |
| Nulliparity | 16 (57.1) | 8 (40.0) | 180 (58.4) | 0.271b) |
| Pre-pregnancy weight (kg) | 54.6±2.1 | 58.5±3.1 | 56.6±0.6 | 0.498a) |
| Maternal weight at delivery (kg) | 63.0±1.9 | 70.3±3.0 | 68.9±0.6 | 0.023a) |
| Cesarean section | 15 (53.6) | 20 (100) | 178 (57.8) | 0.001b) |
| Male sex | 20 (71.4) | 14 (70.0) | 160 (51.9) | 0.050b) |
| Birth weight (kg) | 2.23±0.60 | 2.01±0.86 | 3.15±0.39 | <0.001a) |
| AS<4 at 1 min | 2 (7.1) | 5 (25.0) | 4 (1.3) | <0.001b) |
| AS<7 at 5 min | 2 (7.1) | 2 (10.0) | 3 (1.0) | 0.002b) |
| Parameter | Group 1 (n=28) | Group 2 (n=20) | Group 3 (n=308) | p-valuea) |
|---|---|---|---|---|
| WBC (×103/mm3) | 9.17±2.10 | 9.47±1.55 | 9.52±2.12 | 0.697 |
| PLT (×103/mm3) | 237.75±51.48 | 210.50±53.66 | 237.74±58.53 | 0.124 |
| Neutrophil (×103/mm3) | 6.85±1.75 | 7.31±1.64 | 7.30±2.10 | 0.493 |
| Lymphocyte (×103/mm3) | 1,71±0.44 | 1.58±0.43 | 1.70±0.70 | 0.707 |
| Monocyte (×103/mm3) | 0.41±0.15 | 0.40±0.13 | 0.44±0.46 | 0.854 |
| NLR | 4.17±1.22 | 5.12±2.28 | 4.59±1.66 | 0.150 |
| LMR | 4.45±1.52 | 4.55±2.50 | 4.42±2.40 | 0.968 |
| PLR | 140±38 | 155±54 | 149±49 | 0.533 |
- 1. Eo WK, Kim KH, Park EJ, Kim HY, Kim HB, Koh SB, et al. Diagnostic accuracy of inflammatory markers for distinguishing malignant and benign ovarian masses. J Cancer 2018;9:1165–72.ArticlePubMedPMC
- 2. Kemal Y, Yucel I, Ekiz K, Demirag G, Yilmaz B, Teker F, et al. Elevated serum neutrophil to lymphocyte and platelet to lymphocyte ratios could be useful in lung cancer diagnosis. Asian Pac J Cancer Prev 2014;15:2651–4.ArticlePubMedPDF
- 3. Prodromidou A, Andreakos P, Kazakos C, Vlachos DE, Perrea D, Pergialiotis V. The diagnostic efficacy of platelet-to-lymphocyte ratio and neutrophil-to-lymphocyte ratio in ovarian cancer. Inflamm Res 2017;66:467–75.ArticlePubMedPDF
- 4. Lian L, Xia YY, Zhou C, Shen XM, Li XL, Han SG, et al. Application of platelet/lymphocyte and neutrophil/lymphocyte ratios in early diagnosis and prognostic prediction in patients with resectable gastric cancer. Cancer Biomark 2015;15:899–907.ArticlePubMed
- 5. Temur I, Kucukgoz Gulec U, Paydas S, Guzel AB, Sucu M, Vardar MA. Prognostic value of pre-operative neutrophil/lymphocyte ratio, monocyte count, mean platelet volume, and platelet/lymphocyte ratio in endometrial cancer. Eur J Obstet Gynecol Reprod Biol 2018;226:25–9.ArticlePubMed
- 6. Li A, Yang S, Zhang J, Qiao R. Establishment of reference intervals for complete blood count parameters during normal pregnancy in Beijing. J Clin Lab Anal 2017;31:e22150.ArticlePubMedPMC
- 7. Gomez-Lopez N, StLouis D, Lehr MA, Sanchez-Rodriguez EN, Arenas-Hernandez M. Immune cells in term and preterm labor. Cell Mol Immunol 2014;11:571–81.ArticlePubMedPMCPDF
- 8. Sargin MA, Yassa M, Taymur BD, Celik A, Ergun E, Tug N. Neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios: are they useful for predicting gestational diabetes mellitus during pregnancy? Ther Clin Risk Manag 2016;12:657–65.ArticlePubMedPMC
- 9. Mertoglu C, Gunay M. Neutrophil-lymphocyte ratio and platelet-lymphocyte ratio as useful predictive markers of prediabetes and diabetes mellitus. Diabetes Metab Syndr 2017;11(Suppl 1):S127–31.ArticlePubMed
- 10. Gogoi P, Sinha P, Gupta B, Firmal P, Rajaram S. Neutrophil-to-lymphocyte ratio and platelet indices in pre-eclampsia. Int J Gynaecol Obstet 2019;144:16–20.ArticlePubMed
- 11. Oylumlu M, Ozler A, Yildiz A, Oylumlu M, Acet H, Polat N, et al. New inflammatory markers in pre-eclampsia: echocardiographic epicardial fat thickness and neutrophil to lymphocyte ratio. Clin Exp Hypertens 2014;36:503–7.ArticlePubMed
- 12. Daglar HK, Kirbas A, Kaya B, Kilincoglu F. The value of complete blood count parameters in predicting preterm delivery. Eur Rev Med Pharmacol Sci 2016;20:801–5.PubMed
- 13. Taylan M, Demir M, Kaya H, Selimoglu Sen H, Abakay O, Carkanat AI, et al. Alterations of the neutrophil-lymphocyte ratio during the period of stable and acute exacerbation of chronic obstructive pulmonary disease patients. Clin Respir J 2017;11:311–7.ArticlePubMed
- 14. Yasar Z, Buyuksirin M, Ucsular FD, Kargi A, Erdem F, Talay F, et al. Is an elevated neutrophil-to-lymphocyte ratio a predictor of metabolic syndrome in patients with chronic obstructive pulmonary disease? Eur Rev Med Pharmacol Sci 2015;19:956–62.PubMed
- 15. Qiu Y, Wen Y, Li G, Tao Z, Yan X, Zang N, et al. Maternal neutrophil-to-lymphocyte ratio as a prognostic biomarker for placental inflammatory response in late pregnancy. Nan Fang Yi Ke Da Xue Xue Bao 2018;38:1131–4.PubMedPMC
- 16. Gezer C, Ekin A, Solmaz U, Sahingoz Yildirim AG, Dogan A, Ozeren M, et al. Identification of preterm birth in women with threatened preterm labour between 34 and 37 weeks of gestation. J Obstet Gynaecol 2018;38:652–7.ArticlePubMed
- 17. Chandra S, Tripathi AK, Mishra S, Amzarul M, Vaish AK. Physiological changes in hematological parameters during pregnancy. Indian J Hematol Blood Transfus 2012;28:144–6.ArticlePubMedPMCPDF
- 18. Goto W, Kashiwagi S, Asano Y, Takada K, Takahashi K, Hatano T, et al. Predictive value of lymphocyte-to-monocyte ratio in the preoperative setting for progression of patients with breast cancer. BMC Cancer 2018;18:1137.ArticlePubMedPMCPDF
- 19. Wang QX, Li SH, Ji BY, Wang HY, Li YY, Feng LL, et al. Lymphocyte/monocyte ratio is a novel predictor for early stage extranodal natural killer/T-cell lymphoma, nasal type. J Cancer 2017;8:1030–7.ArticlePubMedPMC
- 20. Zhu JY, Liu CC, Wang L, Zhong M, Tang HL, Wang H. Peripheral blood lymphocyte-to-monocyte ratio as a prognostic factor in advanced epithelial ovarian cancer: a multicenter retrospective study. J Cancer 2017;8:737–43.ArticlePubMedPMC
- 21. Charach G, Rogowski O, Karniel E, Charach L, Grosskopf I, Novikov I. Monocytes may be favorable biomarker and predictor of long-term outcome in patients with chronic heart failure: a cohort study. Medicine (Baltimore) 2019;98:e17108.ArticlePubMedPMC
- 22. Feng F, Zheng G, Wang Q, Liu S, Liu Z, Xu G, et al. Low lymphocyte count and high monocyte count predicts poor prognosis of gastric cancer. BMC Gastroenterol 2018;18:148.ArticlePubMedPMCPDF
References
Figure & Data
References
Citations

- Relationship between Platelet-to-Lymphocyte Ratio and Lymphocyte-to-Monocyte Ratio with Spontaneous Preterm Birth: A Systematic Review and Meta-analysis
Liang Peng, Baodi Cao, Fangpeng Hou, Baolin Xu, Hong Zhou, Luyi Liang, Yu Jiang, Xiaohui Wang, Jingjian Zhou, Lingzhang Meng
Journal of Immunology Research.2023; 2023: 1. CrossRef - High Apoptotic Index in Amniotic Membrane of Pregnant Women is A Risk Factor for Preterm Labor
Anak Agung Gede Putra Wiradnyana, Anak Agung Ngurah Jaya Kusuma, Anak Agung Ngurah Anantasika, I Made Darmayasa, Ryan Saktika Mulyana, Gde Bagus Rizky Kornia
European Journal of Medical and Health Sciences.2023; 5(3): 79. CrossRef - Evaluation of Complete Blood Cell Count Parameters in the Diagnosis of Threatened Preterm Labor and Premature Rupture of Membranes
Jule Eriç Horasanlı, Elifsena Canan Alp, Ramazan Bülbül
Dubai Medical Journal.2022; 5(3): 157. CrossRef - The Association of Inflammatory Biomarker of Neutrophil-to-Lymphocyte Ratio with Spontaneous Preterm Delivery: A Systematic Review and Meta-analysis
Sina Vakili, Parham Torabinavid, Reza Tabrizi, Alireza Shojazadeh, Nasrin Asadi, Kamran Hessami, Oleh Andrukhov
Mediators of Inflammation.2021; 2021: 1. CrossRef

 E-Submission
E-Submission Yeungnam University College of Medicine
Yeungnam University College of Medicine PubReader
PubReader ePub Link
ePub Link Cite
Cite